Naturopathic and Holistic Perspectives on Understanding and Healing Lupus
Lupus: Uncovering Hidden Causes and Holistic Paths to Healing
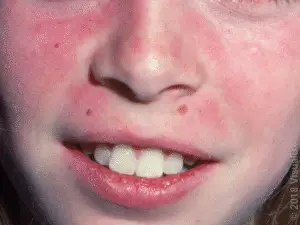
A classic “butterfly” rash across the cheeks and nose (malar rash) in a person with lupus. About 70–80% of lupus patients develop skin rashes, and in 20% of cases a rash like this is the first noticeable sign of the diseasegoodrx.com.
Introduction: A Mysterious Disease Beyond Autoimmunity
Lupus is a chronic disease in which the body’s immune system attacks its own healthy tissues, causing inflammation and damage in multiple organslupus.orghealthline.com. Mainstream medicine classifies lupus as an autoimmune disorder – meaning the immune system is misdirected against the self – and it is typically managed with immunosuppressive drugs rather than curedmfm.aumfm.au. Patients, mostly women of childbearing age, often experience a wide range of symptoms: from joint pain and debilitating fatigue to rashes like the hallmark “butterfly” rash on the face and even life-threatening organ complicationshealthline.comhealthline.com. Despite decades of research, Western medicine has not discovered a definitive cause or a cure for lupus, and treatments largely aim to control symptoms by tamping down the immune systemmfm.aumfm.au. This symptom-focused approach can bring relief, but many lupus sufferers continue to have flare-ups and disease progression, prompting a search for deeper explanations and solutions.
Increasingly, patients and integrative health experts are looking beyond autoimmunity itself to ask why the immune system goes rogue in the first place. Could lupus be the visible tip of an iceberg, underpinned by hidden factors that mainstream medicine has overlooked? There is a growing belief among naturopathic and holistic practitioners that lupus is not simply the body inexplicably “attacking itself,” but rather a syndrome of underlying causes – including chronic infections (pathogens), toxin accumulation, heavy metal exposure, gut imbalances, and even unresolved emotional trauma. In this view, lupus is the body’s reaction to a perfect storm of burdens, and addressing those root causes could alleviate or even reverse the disease process. So far, Western pharmaceutical approaches have failed to provide a true cure or long-term solution for lupus. This has left room for alternative perspectives that incorporate natural, functional, and traditional medicines – as well as emotional and spiritual healing – in hopes of not just managing lupus, but truly healing it.
In this article, we dive deep into lupus from a holistic standpoint. We’ll explore the overlooked triggers and contributors to lupus symptoms, from stealthy viral infections to toxic heavy metals, and discuss how these factors might be the keys to understanding the disease. We will also examine how lupus compares to related conditions like Lyme disease and fibromyalgia – questioning whether these labels are distinct or part of a continuum of illness with common roots. Finally, we’ll highlight naturopathic and integrative approaches for lupus, including detoxification, nutrition, herbal medicine, Traditional Chinese Medicine, Ayurveda, homeopathy, and mind-body therapies. Our goal is to present a neutral, evidence-informed discussion that empowers readers with knowledge of why lupus happens and how a holistic strategy could complement conventional care. While lupus is a complex and serious condition, emerging research and traditional wisdom together suggest new hope: that by looking in the “wrong direction” – the direction mainstream medicine has largely neglected – we might find better ways to truly heal this illness.
The Many Faces of Lupus: Beyond One Disease
The term “lupus” actually refers to a family of related conditions rather than a single disease. The most common and serious form is Systemic Lupus Erythematosus (SLE), which is usually what people mean by “lupus.” SLE is a systemic autoimmune condition in which the immune system can attack virtually any organ or tissue in the body – skin, joints, kidneys, heart, lungs, brain, and moremfm.auhealthline.com. Patients with SLE suffer periods of illness (flares) with symptoms like joint pain, fevers, profound fatigue, rashes, and internal organ inflammation, alternating with remissions where symptoms subsidemfm.aumfm.au. SLE is unpredictable and potentially life-threatening if vital organs (like kidneys in lupus nephritis, or the brain in neuropsychiatric lupus) are affected.
In addition to SLE, there are other forms of lupus that mainly impact specific parts of the body. Cutaneous Lupus refers to lupus limited to the skin. The classic variant is Discoid Lupus Erythematosus (DLE), which causes persistent scaly disk-shaped lesions on sun-exposed areas like the face and scalpmfm.aumedicalnewstoday.com. Discoid lesions can cause scarring and even permanent hair loss if they occur on the scalpmedicalnewstoday.comgoodrx.com. There is also Subacute Cutaneous Lupus, which causes more widespread skin rashes (often ring-shaped or psoriasis-like) that are very photosensitive but typically do not scarmedicalnewstoday.com. Notably, about 5–10% of people with purely cutaneous lupus can eventually develop systemic lupusmfm.aumfm.au, indicating these conditions are on a spectrum.
Another form, Drug-Induced Lupus, is a transient lupus-like syndrome triggered by certain medications. Dozens of drugs (for example, some blood pressure or anti-seizure medications, and the antibiotic minocycline) have been known to cause lupus symptoms in susceptible individualsmfm.aumfm.au. The good news is that drug-induced lupus usually resolves once the offending drug is discontinued. There is also a rare condition called Neonatal Lupus, in which infants of mothers with lupus are born with some lupus-like symptoms (such as a skin rash or temporary heart rhythm disturbances). Neonatal lupus is caused by the mother’s autoantibodies crossing the placenta; it is generally temporary, and the symptoms in the baby often resolve within a few months after birth as the maternal antibodies degrademfm.au.
While these lupus variants each have unique features, they share a common thread: an immune system that has gone awry, leading to inflammation and tissue damage. Conventional medicine acknowledges that genetics play a role across all forms of lupus, and that environmental triggers can tip the balance in a predisposed personlupus.orgmfm.au. However, conventional explanations often stop there – “genes plus something in the environment causes autoimmunity.” From a holistic perspective, we ask: What are those environmental and internal triggers, and why does the immune system become so unbalanced? To answer that, we must shine a light on factors lurking behind the scenes of lupus – factors mainstream research is only beginning to understand.
Conventional Treatment: Managing Symptoms Without a Cure
Before exploring the hidden causes, it’s important to recognize the current standard of care and its limitations. Mainstream medicine treats lupus primarily as an autoimmune inflammatory disease – the focus is on suppressing the overactive immune response to prevent damage to organs. There is indeed no medical cure for lupus at present, so rheumatologists aim to control symptoms and prevent flaresmfm.aumfm.au. Common medications include nonsteroidal anti-inflammatory drugs (NSAIDs) for pain, corticosteroids like prednisone to rapidly quell inflammation, and antimalarial drugs such as hydroxychloroquine (Plaquenil) which help reduce flares and skin/joint symptomsmfm.au. In more severe cases, patients are prescribed immunosuppressants or chemotherapy-type drugs (for example, azathioprine, mycophenolate, cyclophosphamide, methotrexate) to broadly dampen immune activitymfm.aumfm.au. Newer biologic drugs like belimumab (an antibody that reduces certain immune cells) have also been developed specifically for lupus. These treatments can be effective at reducing tissue inflammation and are often life-saving, especially in organ-threatening lupus.
However, these therapies treat the symptoms (inflammation and autoantibodies) rather than the underlying cause of the autoimmunity. As a result, they must often be taken long-term, and many have significant side effectsmfm.aumfm.au. For instance, corticosteroids can cause weight gain, bone loss, and increased infection risk; immunosuppressants carry risks of infections and even cancers due to dampening the immune surveillance. Additionally, even with the best available care, many lupus patients continue to experience disease flares triggered by factors like stress, infections, or sunlight. It’s not uncommon for patients to feel that “Western medicine is just putting a band-aid on the problem,” keeping lupus at bay but never truly restoring full health. The Lupus Foundation of America frankly states that current conventional treatments do not address whatever causes lupus – they only manage the resulting inflammationmfm.au. This reality has driven interest in complementary approaches that might fill the gap.
So far, big pharmaceutical research has largely targeted the immune system itself, trying to modulate or block pathways involved in lupus (for example, B cells that produce autoantibodies, or interferon chemicals that drive inflammation). Yet the cure remains elusive, suggesting we may be looking in the wrong place. What if, as some integrative doctors argue, lupus is not the beginning of the story but rather the result of other processes in the body? To find a true solution, we may need to step back and ask: Why is the immune system so disturbed? The following sections will explore evidence pointing to chronic infections, toxins, and other stressors as root causes that mainstream medicine has only partially acknowledged. By understanding these, we can then discuss holistic strategies – from detoxification to herbal medicine – aimed at correcting the underlying imbalance, not just suppressing the immune system.
Hidden Cause #1: Pathogens and Chronic Infections – The “Stealth” Invaders
One of the most compelling yet under-addressed pieces of the lupus puzzle is the role of infections. For decades, researchers have observed links between certain pathogens and lupus. In fact, exposure to infections is listed among the known environmental triggers for lupus flares and onsetlupus.orglupus.org. For example, the Epstein–Barr Virus (EBV) – the virus that causes mononucleosis – has a well-documented association with lupus. Nearly everyone encounters EBV in their lifetime, but studies show a striking pattern: people with lupus are far more likely to have had EBV and to have high levels of EBV in their bodies than the general populationlupus.orglupus.net. A strong association between EBV infection and systemic lupus has been known since the 1970sthe-rheumatologist.org. More recent research has illuminated possible mechanisms: a 2018 study found that an EBV protein (EBNA2) can attach to human DNA at sites linked to lupus and other autoimmune diseases, potentially flipping immune-related genes on or offlupus.net. In 2021, another team confirmed that EBV can trigger autoimmune reactions seen in lupus, and that EBV tends to reactivate (flare up) more often in lupus patients than in otherslupus.net. In short, the virus may be awakening the sleeping dragon of autoimmunity – either by direct molecular mimicry (virus particles resembling human proteins and confusing the immune system) or by chronically overstimulating the immune system.
EBV is not the only microbial suspect. Other viruses like cytomegalovirus (CMV), parvovirus B19, and even new viruses such as SARS-CoV-2 have been investigated for links to lupusmfm.au. The evidence for these is less extensive than for EBV, but case reports and small studies have suggested, for instance, that parvovirus infection can precede a lupus onset in some patients, and recently scientists have been examining whether COVID-19 (SARS-CoV-2) might trigger autoimmune syndromes in predisposed individualsmfm.au. On the bacterial front, researchers have noted that certain bacterial infections can provoke autoimmunity. For example, Helicobacter pylori (a stomach ulcer germ) and Mycobacterium tuberculosis have been associated with autoantibody production in some studies. More directly relevant to lupus, the gut microbiome appears to play a role: one study found that lupus patients (especially those with lupus kidney disease) had an overgrowth of a specific gut bacterium, Ruminococcus gnavus, at five times the levels found in healthy peoplemfm.aumfm.au. Intriguingly, R. gnavus is known to produce molecules that can breach the gut lining and stimulate immune cells. This suggests a leaky gut and dysbiosis (microbial imbalance) might contribute to lupus by continuously activating the immune system. Other gut bacteria like Proteus, Klebsiella, and Citrobacter species have also been linked to autoimmune reactionsmfm.au, echoing findings in diseases like rheumatoid arthritis.
Perhaps the most striking evidence of an infection triggering lupus comes from observations around Lyme disease. Lyme disease, caused by the bacteria Borrelia burgdorferi from tick bites, is not considered an autoimmune disease per se – it’s an active infection. Yet, chronic or late-stage Lyme can closely mimic autoimmune disorders, and reports have emerged of Lyme infection actually kickstarting lupus in some patientspmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov. In one case, a 35-year-old woman developed full-blown SLE just months after a Lyme infection; her doctors believe the Borrelia infection was the likely trigger for lupus in that casepmc.ncbi.nlm.nih.gov. The proposed mechanism is that long-term exposure to the Lyme spirochete can induce de novo autoimmune disease – essentially, the infection persistently revs up the immune system and eventually causes it to lose tolerance to the body’s own tissuespmc.ncbi.nlm.nih.gov. Chronic Lyme disease patients sometimes continue to have joint pain, fatigue, and even autoantibodies after the bacteria are supposedly cleared, indicating an autoimmune process gets set in motionvibrant-wellness.comvibrant-wellness.com. Borrelia bacteria also have antigens that resemble human proteins, so the antibodies generated against the infection may “cross-react” with the body – a phenomenon known as molecular mimicryvibrant-wellness.comvibrant-wellness.com. This cross-reactivity can potentially lead to conditions like lupus or rheumatoid arthritis being triggered or exacerbated by Lyme diseasevibrant-wellness.comvibrant-wellness.com. In fact, researchers have noted that diagnosing lupus vs. chronic Lyme can be tricky because their symptoms overlap so much, and in some cases an underlying Lyme infection may be mistaken for lupus or vice versapmc.ncbi.nlm.nih.govvibrant-wellness.com. These intersections underscore that infections and autoimmunity are deeply intertwined.
Beyond specific viruses and bacteria, holistic practitioners often talk about “pathogen load” – the cumulative burden on the body from multiple infectious agents (viruses, bacteria, yeasts, parasites) that may be quietly residing in tissues. The idea is that one infection might not be enough to trigger lupus in a resilient person, but if someone accumulates several chronic infections over time, the immune system can become overwhelmed or dysregulated. For example, a person could carry Epstein-Barr virus, have an overgrowth of Candida yeast in the gut, and also harbor bacteria like Mycoplasma or Chlamydia – none of these alone causes lupus in everyone, but together they create constant immune stimulation. At some tipping point, the theory goes, the immune system shifts into an autoimmune mode. There is some evidence to support this concept: lupus patients often have higher levels of antibodies indicating past or chronic infections. One study noted lupus patients had abnormal responses to common gut bacteria as if their immune tolerance was brokenmfm.au. Another line of evidence is that flares of lupus frequently follow infections. It’s well known clinically that a simple infection can trigger a lupus flare, and lupus.org lists infections (like a cold or flu) as a top environmental trigger for symptom flareslupus.org. Rather than viewing that as just “stress on the body causing a flare,” it could be that the flare is the immune system’s overreaction to the infection, made possible by prior immune dysregulation.
So, how can this knowledge guide us? If lupus has a significant infectious component, then addressing those hidden infections could be key to improving health – a vastly different approach than solely giving immunosuppressants. Some integrative physicians, for example, will test lupus patients for chronic active Epstein-Barr virus or for Lyme disease and co-infections. If found, treatments might include long-term antivirals, antimicrobial herbs, or even antibiotics to reduce the pathogen load. There are intriguing anecdotal reports of lupus patients going into remission when a chronic infection is successfully treated. One famous unconventional theory by writer “Medical Medium” even posits that lupus is caused by EBV feeding off toxins – while that particular interpretation is not scientifically proven, it underscores the perceived centrality of pathogens and toxins acting together. Indeed, researchers have noted that infections can make the body more vulnerable to toxins: “Through immunomodulation, pathogens can compromise the immune system and increase sensitivity to environmental pollutants and toxins,” as one review on autoimmunity statedvibrant-wellness.comvibrant-wellness.com. In other words, infections and toxins can act in concert to break down our defenses. This brings us to the next hidden factor in lupus – one that often works hand-in-hand with infections – toxic exposures and heavy metals.
Hidden Cause #2: Toxins and Heavy Metals – An Invisible Burden
Environmental toxins are everywhere in modern life – in our air, water, food, and products. Mounting evidence suggests that lupus and other autoimmune diseases are linked to cumulative toxic exposures. Heavy metals in particular have drawn concern. Mercury, lead, cadmium, arsenic, and other metals are known to be toxic to the immune system, and researchers have observed that people with high exposure to these metals can develop lupus-like autoimmunitypmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov. For instance, mercury exposure (such as in certain mining occupations or possibly through mercury amalgam dental fillings) has been associated with a higher prevalence of antinuclear antibodies (ANAs) – the hallmark autoantibodies of lupuspmc.ncbi.nlm.nih.gov. In one study, gold miners exposed to mercury had significantly more positive ANA tests than miners not exposed to mercurypmc.ncbi.nlm.nih.gov. Two separate case-control studies likewise found that people who self-reported mercury exposure had an elevated risk of SLE compared to unexposed controlspmc.ncbi.nlm.nih.gov. Lead and cadmium, common heavy metals in industrial pollution and cigarette smoke, have also been implicated. Epidemiological data from the Nurses’ Health Study showed that exposure to lead or cadmium (for example, through old leaded paint or industrial sources) correlated with increased lupus risklupus.org. In laboratory models, these metals can provoke autoimmune reactions: mice or cell cultures exposed to cadmium or lead release more inflammatory cytokines and produce abnormal immune responsesdrhilarychambers.com.
How do heavy metals induce autoimmunity? Naturopathic immunologist Dr. Hilary Chambers explains it this way: the immune system may initially respond to the heavy metal particles as foreign invaders, creating immune cells (T-cells and antibodies) specific to the metaldrhilarychambers.com. Normally, the body should eliminate or tolerate these cells if they start reacting to the body itself. But heavy metals interfere with the immune system’s safety checkpoints. Research shows that mercury, for example, prevents the destruction of self-reactive T-cells that should have been eliminateddrhilarychambers.com. In Dr. Chambers’ metaphor, the “soldier” immune cells trained to attack the metal end up going rogue and attacking the body because the metal exposure disrupted the normal training processdrhilarychambers.comdrhilarychambers.com. Additionally, metals like cadmium and lead are known to generate oxidative stress and inflammation; they can directly stimulate the release of inflammatory cytokines (immune signaling molecules)drhilarychambers.com. They also disturb the gut microbiome, as noted in one study – heavy metals can kill beneficial bacteria and promote a dysbiosis, which is significant because a large portion of the immune system is located in the gutdrhilarychambers.comdrhilarychambers.com. All these effects create a pro-autoimmune environment inside the body.
Mainstream research echoes these concerns. A comprehensive review in Nature on lupus risk factors concluded that “heavy metals, such as mercury, are hypothesized to increase risk of SLE”, although definitive proof in humans is still being gatheredpmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov. Mechanistic studies in mice have clearly shown mercury can trigger lupus-like disease in susceptible strainspmc.ncbi.nlm.nih.gov. The Lupus Foundation lists contact with heavy metals like lead and cadmium as environmental factors “very likely” to contribute to lupuslupus.org. Moreover, other toxins like certain chemicals and drugs can cause lupus or lupus-like conditions. Notoriously, chronic exposure to silica dust (as in certain mining, construction, or pottery jobs) is one of the best documented environmental risk factors for lupuspmc.ncbi.nlm.nih.gov. Silica particles can lodge in the lungs and trigger ongoing inflammation, and studies consistently find higher lupus rates in people exposed to silica (one reason lupus is an occupational hazard in some industries)lupus.org. Pesticides and solvents have also been linked to higher lupus incidence in several studiespmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov. One large study found women with frequent pesticide exposure had over twice the odds of developing lupus compared to those with no such exposurepmc.ncbi.nlm.nih.gov. These toxins can act synergistically: interestingly, animal research suggests that co-exposure to multiple heavy metals or to metals plus other toxins can amplify the autoimmune response beyond each factor alonevibrant-wellness.comvibrant-wellness.com.
From a holistic viewpoint, the body’s toxic load is a crucial piece of the lupus puzzle. Our liver and kidneys are responsible for detoxifying many harmful substances, but if someone’s exposure is high or their detox pathways are sluggish (due to genetics or nutrient deficiencies), toxins accumulate in tissues. Heavy metals may hide in fat, bones, or even in the brain, persisting for years. Could this toxic burden continuously irritate the immune system, leading to lupus symptoms? Many naturopathic doctors think so. They often test lupus patients for heavy metal levels – using hair analysis, blood tests, or provoked urine tests where a chelating agent is given to draw metals out of storagedrhilarychambers.comdrhilarychambers.com. It’s not uncommon for such testing to reveal elevated mercury or lead in patients who never suspected exposure (sources can range from old amalgam dental fillings, to eating a lot of big ocean fish high in mercury, to living in a polluted urban area or an older home with lead paint). In those cases, a targeted detoxification plan might be implemented. This can include medically supervised chelation therapy (using compounds like DMSA or EDTA to bind metals) for the most severe toxicitydrhilarychambers.com. Or, more gentle naturopathic approaches might be used, such as supplements and foods that support the body’s own detox systems. For example, nutrients like N-acetyl cysteine (NAC), selenium, and B-complex vitamins help boost glutathione and other liver detox pathwaysdrhilarychambers.com. Herbs like milk thistle can support liver function, and antioxidants like vitamin C and alpha-lipoic acid can help neutralize oxidative damage from metalsdrhilarychambers.comdrhilarychambers.com. Natural chelators and binders are also used – these include things like modified citrus pectin, chlorella, cilantro (coriander), and spirulina, which have some ability to bind metals and carry them out of the bodydrhilarychambers.comdrhilarychambers.com.
Mercury (Hg), lead (Pb), cadmium (Cd) and other heavy metals on the periodic table. Heavy metal exposure – through sources like dental amalgams, contaminated food, smoking, or pollution – has been linked to immune system dysregulation and lupus in researchpmc.ncbi.nlm.nih.govlupus.org. Integrative medicine approaches often include detoxifying these metals to help calm autoimmunity.
The principle of detoxification is a cornerstone of naturopathic and traditional healing systems when addressing chronic diseases like lupus. The rationale is simple: if the disease is fueled by toxins (whether external like metals and pesticides, or internal like waste products of pathogens), then removing those toxins can lighten the load on the immune system and allow the body to heal. There is anecdotal evidence of lupus patients who improve significantly after aggressive detox interventions. For instance, one case study in a naturopathic journal described a woman with lupus who underwent an Ayurvedic Panchakarma (a deep detox program involving diet, herbal medicines, and therapies like oil massage, steam, and cleansing enemas) – after this detox and lifestyle regimen, she achieved remission of lupus symptoms and her lab markers normalized, without other medications. Such reports are not yet backed by large clinical trials, but they align with the experiences of some integrative clinicians. Dr. Chambers emphasizes in her article that heavy metal detox can “help to slow or reverse the disease process because it addresses one of the underlying causes” of autoimmunitydrhilarychambers.com. Conventional doctors might be skeptical of these claims, but given that standard treatments do not cure lupus, it is understandable that patients explore these options. Of course, any detox should be done safely and ideally under guidance – some detox methods (like improper chelation) can be risky if done incorrectly. But supporting the body’s natural elimination routes – drinking clean water, eating fiber to bind toxins in the gut, sweating via exercise or sauna, and taking liver-supportive nutrients – is generally low-risk and can be beneficial for overall health.
To summarize, heavy metals and toxins act as immune system agitators that can push a susceptible person into lupus. They also may work together with infections: for example, a virus might impair the immune system’s ability to clear a toxin, or a toxin might weaken the body’s defense against infectionsvibrant-wellness.com. This dual attack can overwhelm our system’s balance (the field of toxicology even has a concept called the “two-hit hypothesis” – you need two insults to cause autoimmunity, say a genetic predisposition plus an environmental toxin). In lupus, we see multiple hits: genes, an infection, a heavy metal, stress – all layering. The encouraging news is that unlike genes, infections and toxins are potentially modifiable factors. We can treat infections; we can detoxify metals; we can reduce pesticide exposure. This means a lupus patient is not wholly at the mercy of fate or immunosuppressants – there are concrete actions to identify and remove triggers, which many holistic practitioners report can lead to significant improvement.
Hidden Cause #3: The Leaky Gut and Food Connections
Hippocrates said, “All disease begins in the gut,” and modern research is finding that autoimmune diseases indeed have deep roots in gut health. Lupus is no exception. A growing area of interest is the gut microbiome and intestinal permeability (aka “leaky gut”) in lupus. We touched on how lupus patients have an overgrowth of certain gut bacteria like Ruminococcus gnavus which can provoke immune responsesmfm.au. Additionally, lupus patients have been found to often harbor less of certain beneficial bacteria such as Bacteroides uniformis, which normally help keep the immune system calmmfm.au. A dysregulated microbiome can lead to a compromised gut lining, where the junctions between intestinal cells become “leaky.” This allows bacterial fragments and dietary proteins that should stay in the gut to seep into the bloodstream, stimulating the immune system. In lupus, scientists have observed markers of leaky gut and higher levels of bacterial endotoxins in the blood, suggesting that gut barrier dysfunction may fuel systemic inflammationmfm.au.
Food itself can also be a trigger for immune reactions in sensitive individuals. Many people with autoimmune conditions, including lupus, report that certain foods exacerbate their symptoms. Common culprits are gluten (the protein in wheat and related grains) and dairy. Interestingly, the functional medicine perspective notes that celiac disease (an autoimmune disease to gluten) and lupus can co-occur, and gluten sensitivity might worsen lupus flares in some patientsmfm.au. Some preliminary research hints that a subset of lupus patients have antibodies that cross-react with wheat or milk proteins, which could mean those foods aggravate the autoimmune process. At Melbourne Functional Medicine, practitioners often recommend lupus patients try an elimination diet – removing common inflammatory foods like gluten, dairy, refined sugar, and sometimes nightshade vegetables – to see if symptoms improvemfm.aumfm.au. They also test for food sensitivities or allergies, which, if present, can drive immune dysfunction. By identifying and eliminating reactive foods, the overall inflammatory burden can be reduced.
Furthermore, nutritional deficiencies can play a role in autoimmunity. Vitamin D is a famous example: it’s a vitamin that doubles as an immune-regulating hormone. Low vitamin D levels are linked with higher autoimmune disease risk, and in lupus many patients are vitamin D deficient (sometimes due to avoiding sun exposure, which lupus patients must do to prevent rashes). Adequate vitamin D is necessary for immune tolerance, and deficiency might remove a check on autoimmunitymfm.au. Supplementing vitamin D has been shown in some studies to help reduce lupus disease activity modestly. Omega-3 fatty acids (from fish oil or flax) are another important nutrient; they have anti-inflammatory effects that could counter the rampant inflammation in lupus. Small trials have found fish oil supplements can lower certain inflammatory markers in lupus. Selenium and magnesium are also often recommended by integrative practitioners for lupus to support antioxidant defenses and reduce inflammationmfm.aumfm.au.
From a holistic standpoint, healing the gut is a foundational step in treating lupus. This often involves a multipronged approach: removing irritants (like allergenic foods, alcohol, or certain medications that harm the gut lining), eradicating any overgrown harmful microbes (such as Candida yeast or parasites – integrative doctors may test stool samples for thesemfm.au), and then restoring a healthy gut environment. Restoration includes eating a high-fiber, whole-food diet to feed beneficial bacteria, possibly taking probiotics (supplemental friendly bacteria), and using gut-healing nutrients. Supplements like glutamine (an amino acid that nourishes intestinal cells), zinc, and omega-3s can help repair the gut barrier. Herbal remedies like slippery elm, aloe vera, or deglycyrrhizinated licorice are also used in natural medicine to soothe and heal the gut lining. The functional medicine program in Melbourne explicitly tests lupus patients for “leaky gut,” dysbiosis, SIBO (small intestinal bacterial overgrowth), and Candida as part of their work-upmfm.aumfm.au. If those tests come back positive, they target those problems with personalized protocols – e.g. antimicrobial herbs or medications for SIBO, antifungal agents for Candida, and then probiotics and diet changes.
All of this gut talk circles back to the notion that the immune system’s balance is heavily influenced by what’s happening in our digestive tract. About 70% of the body’s immune cells reside in gut-associated lymph tissuedrhilarychambers.com. If the gut is constantly exposed to unwelcome substances (be it improperly digested food, bacterial toxins, or heavy metals we ingest), the immune cells there may become hyperactive and start misbehaving, potentially sparking systemic autoimmunity. On the flip side, a well-functioning gut can produce short-chain fatty acids and other metabolites that calm inflammation and promote regulatory immune cells.
In summary, paying attention to diet and gut health is not just “alternative fluff” – it’s increasingly recognized as a critical piece of autoimmunity. Even if mainstream rheumatologists don’t prescribe probiotics or gluten-free diets routinely, many will agree that eating an anti-inflammatory diet (rich in vegetables, fruits, omega-3s, etc.) and avoiding junk food is beneficial for lupus patients. A Lupus Foundation article notes that ultra-processed foods high in sugar and additives may worsen inflammation and are best minimizedlupus.org. Indeed, they list eating ultra-processed foods as a potential lupus trigger alongside toxins. The holistic approach takes it further by identifying specific food intolerances and gut infections and correcting them. Many patients who adopt these changes report not only fewer lupus flares but better digestion, energy, and mood – because a healthier gut translates to better overall health.
Hidden Cause #4: Stress and Trauma – The Mind-Body Connection
While viruses and heavy metals are tangible triggers, lupus is also closely tied to less tangible factors: psychological stress and emotional trauma. It has long been observed that lupus flares often follow periods of intense stress. Patients frequently report that their first lupus symptoms began after a major life event like a divorce, the loss of a loved one, or another traumatic incident. Now, scientific research is validating these anecdotes. A landmark study by Harvard researchers in 2017 found that women who had experienced severe trauma and developed post-traumatic stress disorder (PTSD) had nearly a three-fold increased risk of developing lupus compared to women with no trauma historyhsph.harvard.edu. Even women who went through trauma but did not meet full PTSD criteria had more than double the risk of lupus compared to non-traumatized womenhsph.harvard.edu. These are striking numbers, indicating that psychological injury can translate into physical autoimmunity. The lead author of that study, Dr. Andrea Roberts, stated: “There is a lot of research showing that mental health, stress and trauma affect physical health and serious illnesses like lupus. Things going on in our minds really affect our physical health.”hsph.harvard.edu. In other words, the mind-body connection is real and powerful.
Chronic stress – even at levels below clinical PTSD – can worsen lupus. Stress hormones like cortisol and adrenaline can dysregulate the immune response over time. Initially, high cortisol is immunosuppressive (which might seem protective), but with chronic stress the body often develops cortisol resistance or fluctuating levels, which can lead to increased inflammation. Stress can also trigger flares by reactivating latent viruses (for example, EBV tends to reactivate during stress, which could then provoke lupus activity)theforbesclinic.co.ukvibrant-wellness.com. The Lupus Foundation lists emotional stress, including PTSD, as a confirmed trigger that can cause lupus onset or flareslupus.org. Patients with lupus often notice their symptom severity tracks with their stress levels: high stress can bring on joint pains, fatigue, rashes, etc., whereas periods of relaxation might prolong remission.
Beyond the biochemical effects of stress, some theories suggest that emotional factors – such as internalized emotions or past trauma stored in the body – might underlie autoimmune tendencies. There’s a school of thought in mind-body medicine that autoimmune disease could represent the body “attacking itself” in a metaphorical reflection of self-criticism or unhealed emotional wounds. This is more philosophical, but interestingly many lupus patients are noted to be high-achievers or people who carry a lot of responsibility and stress, often ignoring their own needs. An emerging field called psychoneuroimmunology studies how our mental state can alter immune function. Techniques that reduce stress have been shown to have measurable effects on the immune system – for instance, mindfulness meditation has been associated with lower levels of inflammatory markers and may even increase the number of regulatory T-cells (the cells that help keep autoimmunity in check) according to some studies. In lupus specifically, small trials have found mindfulness-based stress reduction can improve patients’ pain and psychological well-beinglupus.orglupus.org. Practices like yoga and Tai Chi, which combine gentle physical activity with relaxation, have also shown benefits: Lupus patients doing Tai Chi reported better mood and coping, and improved flexibility without triggering flareslupus.orglupus.org. These practices likely work by toning down the chronic “fight or flight” response and activating the parasympathetic nervous system, which in turn decreases inflammatory signaling.
Another facet is trauma release. For those with a history of significant trauma, therapies such as psychotherapy (especially cognitive-behavioral therapy or trauma-focused therapy like EMDR), somatic experiencing, or even newer approaches like neurofeedback can help process and release the psychological burden. While directly treating trauma might not be a “cure” for lupus, there are cases where working through deep emotional issues coincided with disease improvement. The mind and immune system communicate via hormones, neurotransmitters, and cytokines, so alleviating chronic emotional distress can create a physiological environment more conducive to healing. As one rheumatologist noted, “Women who have lupus often report stress as a trigger for flares, similar to other autoimmune diseases”the-rheumatologist.org. Recognizing this, comprehensive lupus care should ideally include mental health support – be it counseling, support groups, stress management workshops, or mind-body techniques.
It’s also worth mentioning the spiritual dimension some patients explore. A serious illness like lupus often leads people to re-evaluate their lives, find meaning, and tap into spiritual or community support. Whether through prayer, meditation, or other spiritual practices, many find an improved sense of peace that helps them cope with lupus and possibly influences their health outcomes. No scientific paper can quantify prayer’s effect on lupus, but the reduction in anxiety and the hope that spirituality can provide may indirectly benefit the immune system. The takeaway is that healing from lupus (or any chronic disease) is not just a physical process but also an emotional and spiritual journey. Attending to one’s mental and emotional health is a critical component of a holistic approach. Indeed, some alternative practitioners feel that unhealed emotional trauma is the root cause of lupus in certain cases, more primary than even infections or toxins. They might cite cases where, for example, addressing childhood trauma through therapy led to a dramatic downturn in autoimmune activity. While each person’s case is unique, it underscores that for true healing, all aspects of the person must be considered: body, mind, and spirit.
Holistic Approaches to Lupus: Treating the Whole Person
Given the multitude of factors potentially driving lupus, it’s clear that a successful approach may need to be multi-faceted as well. This is where naturopathic, functional, and traditional medicine approaches come in – they aim to support the entire body’s balance and address root causes, rather than focusing narrowly on suppressing the immune system. Let’s explore some of the key strategies in these holistic approaches:
Detoxification and Internal Cleanse
As discussed, detox is a central concept. In practice, a detox program for lupus might involve steps like: improving diet quality (eliminating processed foods, increasing organic vegetables and fiber to aid natural detoxmfm.aumfm.au), staying well-hydrated, and using specific supplements that enhance liver and kidney function (e.g. NAC, milk thistle, B-vitamins for liver Phase 2 detox, and herbal teas like dandelion or nettle to gently support kidneys). For heavy metals, naturopaths might prescribe natural chelators such as chlorella algae, cilantro, garlic, and fiber like psyllium to bind metals in the gutdrhilarychambers.comdrhilarychambers.com. They may also ensure the patient’s selenium and zinc levels are optimized, as these minerals can help protect the body from mercury and lead toxicity by competing with them and supporting antioxidant enzymes. Sweating therapies – like far-infrared sauna or Epsom salt baths – are sometimes recommended to promote toxin excretion through the skin (with caution and medical clearance, since lupus patients can be sensitive to heat if they have active inflammation). The concept of “drainage” in some herbal traditions (like homeopathic drainage remedies) is also used to gently nudge the body’s elimination pathways.
Anti-Inflammatory Nutrition and Supplementation
Diet is tailored to be anti-inflammatory and nutrient-dense. A common plan might resemble the Mediterranean diet (lots of vegetables, fruits, olive oil, fish, nuts) which has been associated with reduced inflammation. Omega-3 fatty acids from fish oil supplements or flaxseed can help lower inflammation; lupus patients may take a high-quality fish oil daily to support their joints and heart health. Vitamin D3 supplementation is almost routine, since deficiency is so common – doses might range from 2,000 to 5,000 IU daily, adjusted to achieve optimal blood levels (with careful monitoring in case of kidney involvement, since excessive vitamin D can raise calcium levels). Vitamin C, vitamin E (as mixed tocotrienols), and glutathione precursors are given as antioxidants to counteract oxidative stress that fuels lupus flaresmfm.aumfm.au. For example, N-acetyl cysteine (NAC) not only helps detox but also raises glutathione, the body’s master antioxidant; interestingly, one study in lupus nephritis patients found adding 1.8 grams of NAC per day improved kidney function and reduced fatiguepmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov. Magnesium is supplemented to help with muscle pain and stress reduction (magnesium is often low in people with chronic stress). Selenium has dual benefits: it binds mercury and is needed for glutathione enzymes, plus some research suggests it may reduce autoantibody levelsmfm.au.
In terms of herbal medicine, numerous herbs are utilized for their immune-modulating and anti-inflammatory properties. Turmeric (Curcumin) is a star anti-inflammatory herb – it can inhibit NF-kB and other inflammatory pathways, and small trials have shown curcumin can alleviate lupus nephritis symptoms by reducing proteinuria and hematuria. Ginger, green tea (EGCG), and Boswellia (frankincense) are other natural anti-inflammatories that might be included in a lupus protocol. Adaptogenic herbs like Ashwagandha (Withania somnifera) and Rhodiola might be used to support the adrenal glands and stress response, thereby indirectly helping immune balance. In fact, Ashwagandha has immune-modulating effects (it can calm an overactive immune system while boosting an underactive one) and is an important herb in Ayurveda for autoimmune conditionssaiayushayurveda.com. Some practitioners use medicinal mushrooms like reishi or cordyceps, which are known to modulate immunity and reduce autoimmunity in some studies – they must be used carefully, though, as any immune stimulant could, in theory, exacerbate lupus if not balanced.
Traditional Chinese Medicine (TCM) Perspective
Traditional Chinese Medicine offers a very different lens. In TCM, lupus is not labeled as an autoimmune disease but seen as a complex pattern of internal imbalance. Historically, symptoms of lupus might be described by TCM practitioners as syndromes of “Yin deficiency with Heat” or “Blood Heat” and often involving organ systems like the Kidney and Spleen. For example, TCM literature often notes that lupus involves Heat toxins in the blood (to explain fevers and rashes) and Yin deficiency (to explain chronic inflammation and fatigue, as Yin is the cooling, moistening principle of the body)meandqi.commeandqi.com. Yin deficiency in lupus patients might manifest as night sweats, feeling of heat in the palms and soles, and a red peeled tongue – classic TCM signs that the body’s cooling reserve is depletedmeandqi.commeandqi.com. There can also be a Yang deficiency aspect in some lupus cases (especially those with kidney involvement or edema), which corresponds to fatigue, cold hands and feet, and water retentionmeandqi.commeandqi.com.
TCM treatment aims to restore balance. This is done through a combination of acupuncture, herbal medicine, and dietary recommendations. Acupuncture can be used to reduce pain, improve circulation, and calm the mind. Some small studies have suggested acupuncture may help lupus patients by, for instance, improving kidney function in lupus nephritis or reducing arthritis pain, though large evidence is limitedlupus.orglupus.org. It’s generally considered safe if done by a trained practitioner, and many lupus patients use it for symptom management.
The real powerhouse in TCM for lupus is herbal medicine. Chinese herbs are often given in formulas tailored to the patient’s pattern. A classic formula for systemic lupus is Qing Hao Bie Jia Tang, which is traditionally used to nourish Yin and clear Heat from the deeper layers – interestingly, this formula contains sweet wormwood (Qing Hao) which has anti-inflammatory properties, and soft-shelled turtle shell (Bie Jia) which in TCM nourishes Yin; modern studies have found this formula can reduce lupus skin lesions and inflammationmeandqi.commeandqi.com. Another herb, Tripterygium wilfordii (known as Thunder God Vine), has been used in China for autoimmune diseases including lupus; it has potent immunosuppressive compounds and indeed Western science isolated a chemical (triptolide) from it that shows strong anti-inflammatory effects. However, Tripterygium can be toxic to the liver and fertility, so it must be used carefully – in China, refined extracts are used under supervision. TCM doctors also use formulas to strengthen the kidneys and spleen if those are weak – for example, Wu Ling San is a formula that addresses Spleen and Kidney Yang deficiency and helps relieve edema and improve kidney functionmeandqi.com. Many lupus patients in Asia use a combination of Western and Chinese medicine for best resultspmc.ncbi.nlm.nih.gov. Research in China has indicated that integrating TCM herbs with conventional treatment can increase efficacy and reduce side effects of steroids, although quality studies are still neededsciencedirect.com. TCM also advises on lifestyle: lupus patients are counseled to avoid excessive sun (which aligns with Western advice), keep a balanced routine, manage stress (since emotional imbalance can translate into organ imbalance in TCM), and eat a diet based on their constitution – for instance, someone with Heat signs would be told to avoid spicy, fried foods and alcohol, focusing instead on cooling foods like mung beans, pears, and dark leafy greens.
Ayurveda and the Art of Balance
From the Ayurvedic perspective (the traditional medicine of India), lupus can be thought of as a disorder of immune function caused by fundamental imbalances in the doshas (Vata, Pitta, Kapha) and the accumulation of “ama” (toxins or undigested wastes) in the bodysaiayushayurveda.comsaiayushayurveda.com. Ayurveda doesn’t have a historical term for lupus, but it would classify the patient by their symptoms. Many lupus presentations would be seen as involving excess Pitta (the dosha of fire) because of the inflammation, fevers, and rashes (which correspond to heat in the body). At the same time, joint pain and tissue damage might involve Vata (the dosha of air/wind, which when aggravated can cause pain, dryness, and tissue depletion). So an Ayurvedic diagnosis might be something like “Vata-Pitta vyadhi with Ama” meaning an illness caused by deranged Vata and Pitta with toxin buildup. The treatment, therefore, focuses on removing Ama (detoxification) and calming the disturbed doshas.
Ayurvedic detox is famously done through Panchakarma, a series of five cleansing actions. In a lupus context, a Panchakarma retreat might begin with preparatory steps like massage with medicated oils (Abhyanga) and steam therapy (Swedana) to loosen and mobilize toxinssaiayushayurveda.comsaiayushayurveda.com. Then, depending on the patient’s strength, therapies like Virechana (therapeutic purgation) might be used to eliminate excess Pitta and Ama through the bowelsaiayushayurveda.com. Basti (medicated enemas) are often employed, especially to calm Vata and nourish the colon – in fact, Ayurveda considers Basti as one of the most effective treatments for autoimmunity because it can deliver herbs directly to the gut and also balance Vata systematicallysaiayushayurveda.comsaiayushayurveda.com. Through Panchakarma, many patients report significant reduction in symptoms; one case study described a 37-year-old female with 6-year history of lupus who, after a course of Panchakarma and herbal treatment, had reduced pain and was able to taper off steroidspmc.ncbi.nlm.nih.govsukhayuayurved.com.
Ayurvedic herbal remedies for lupus would include immune-modulating and anti-inflammatory herbs known as Rasayanas. Ashwagandha (Withania somnifera) is one such herb, prized for rebuilding strength and calming the mind – it’s often given to autoimmune patients for its adaptogenic qualitiessaiayushayurveda.com. Guduchi (Tinospora cordifolia) is another key herb; it’s sometimes called “amrita” (nectar of immortality) in Ayurveda and has been shown to have anti-inflammatory and immune-normalizing effects. Guduchi is actually the subject of some research in rheumatoid arthritis and has shown benefit, which suggests it could help in lupus as well. Turmeric (Haridra) is heavily used in Ayurveda, often combined with black pepper to enhance absorption; beyond its general anti-inflammatory benefits, turmeric in Ayurveda is said to “purify the blood” which aligns with clearing Ama and soothing Pitta. Other herbs like Triphala (a trio of fruits that aid digestion and detox), Manjishtha (Rubia cordifolia, a blood-purifying herb good for skin conditions), and Shatavari (for nourishing Yin/fluids and female hormones) might be included based on the patient’s needs. Ayurveda also often uses metals/minerals in bhasma form (ash form) for autoimmune diseases, such as a purified calcined formulation of gold or mercury (known as Rasa Shastra medicines). These are complex and must be prepared properly to avoid toxicity – while controversial, some Ayurvedic physicians claim these can dramatically reduce autoimmune activity. The Lupus Foundation, however, cautions that some Ayurvedic products can contain toxic heavy metals if not made correctlylupus.orglupus.org, so one should approach such remedies carefully and under experienced guidance.
Diet and lifestyle in Ayurveda are individualized. Generally, for lupus (which often involves high Pitta), a Pitta-pacifying diet is recommended: this includes cooling, anti-inflammatory foods like leafy greens, cucumbers, coconut water, and spices like fennel and coriander, while avoiding very spicy, sour, or fried foods that aggravate Pittasaiayushayurveda.comsaiayushayurveda.com. To address Vata aspects, warm cooked foods and good fats (like ghee) are included to nourish tissues. Stress reduction is also built into Ayurveda – through yoga, meditation, pranayama (breathing exercises) – which dovetails with what we discussed about trauma and stress. Yoga especially can be gentle or vigorous depending on the patient, but many lupus patients find a slow, restorative yoga practice helps joint stiffness and stress management without overheating the body. Pranayama like alternate-nostril breathing can balance the nervous system and is often taught in Ayurvedic clinics.
One advantage of systems like TCM and Ayurveda is that they offer a framework to tailor treatments to each person’s unique imbalance, rather than a one-size-fits-all approach. A disadvantage is that scientific evidence for these approaches is still limited – but that is changing gradually as more studies are being conducted (for example, trials of Ayurvedic herbs in rheumatoid arthritis have shown positive outcomes). For a patient, the key is to ensure any alternative treatment is complementary to their conventional care, not in conflict. Many patients use these modalities alongside their prescriptions – for instance, staying on hydroxychloroquine and low-dose prednisone while gradually implementing diet changes, herbs, and stress reduction, with the aim of reducing reliance on the harsher drugs over time if possible.
Homeopathy and Energy Medicine
Another holistic modality sometimes used for lupus is homeopathy. Homeopathy is a system from Germany over 200 years old, based on treating patients with highly diluted substances that in larger doses would cause symptoms similar to what the patient has. It’s controversial because the remedies are often diluted beyond Avogadro’s number (meaning no molecules of original substance likely remain), yet some individuals report significant improvements with homeopathic treatment. In lupus, there are case reports of homeopathy leading to remission. For example, a case report published in a homeopathic research journal described a 28-year-old woman with SLE who was not improving with standard drugs; after 2 years of individualized homeopathic remedies (selected based on her unique symptom profile), she recovered clinically, her symptoms subsided, and remarkably her anti-dsDNA antibody – a key lupus marker – turned negativejournals.acspublisher.comjournals.acspublisher.com. The authors reported improved quality of life and no relapses during the follow-upjournals.acspublisher.com. Another case by Indian homeopaths documented improvement in a young girl with discoid lupus using a remedy made from Bacillinum (a homeopathic preparation) along with dietary changeshomeobook.com. While these are not controlled trials and could be placebo or natural remission, they are intriguing. Homeopaths would choose a remedy that matches the person’s totality of symptoms – common remedies for lupus might include Arsenicum album (for those with anxiety, restlessness, burning pains), Apis mellifica (for swelling, redness, and better from cold applications), or Calcarea carbonica (for those with fatigue, cold intolerance, and swollen glands), among many others, depending on the individual. The lupus community should approach homeopathy with open-minded caution: it is safe (no direct side effects due to extreme dilution) but its efficacy is not scientifically established beyond case studies. However, given lupus’ complexity, some patients do explore it. At the very least, a gentle homeopathic remedy could provide symptomatic relief (some patients claim it helps their fatigue or joint pain). If a patient finds benefit, it can be integrated as long as it doesn’t replace essential conventional treatments for severe organ manifestations.
Energy medicine and other spiritual healing practices are also part of some holistic lupus protocols. These can include Reiki (a Japanese energy healing technique), Therapeutic Touch, Qi Gong, or even healing prayer circles. These modalities aim to balance the subtle energy field of the body, which in Eastern terms could be thought of as balancing the life force or Qi. While evidence is anecdotal, some lupus patients feel that regular Reiki sessions reduce their pain and stress. Such therapies likely promote deep relaxation, akin to meditation, which as we know can lower stress hormones and inflammation. There’s essentially no risk to trying these, as long as one continues standard medical monitoring, and they may enhance overall well-being.
Putting It All Together: The Functional Medicine Model
The term Functional Medicine often encapsulates the holistic approach using modern science. A functional medicine practitioner treating lupus will start with an extremely thorough history – looking for all the triggers we’ve discussed. They may order advanced testing: for instance, checking for hidden infections (EBV chronic activation via blood titers, Lyme via Western blot or newer DNA tests, chronic viral load tests), assessing environmental toxin load (such as a urine test for glyphosate or phthalates, a blood test for lead, etc.), running a comprehensive stool analysis to evaluate the gut microbiome, and testing for food sensitivities (like IgG food antibody panels or elimination diet trials)mfm.aumfm.au. They also might do genomic testing for susceptibilities (like the MTHFR gene variant that affects methylation and detox – which was mentioned in the functional medicine list of risk factorsmfm.aumfm.au). All this information creates a matrix of imbalance to be corrected.
The treatment plan in functional medicine is very personalized, but generally it will incorporate all the layers: remove triggers, replenish deficiencies, restore balance. For a lupus patient, a functional doc might implement the “5 R’s of autoimmune healing”: Remove (infections, toxic foods, toxins), Replace (support digestion and hormone balance if needed), Reinoculate (with probiotics for gut health), Repair (nutrients for gut lining and tissue repair), and Rebalance (addressing lifestyle factors like stress, sleep, and exercise). It’s a whole-body approach. As an example, suppose a lupus patient is found to have high mercury, low vitamin D, dysbiosis with candida, and a history of childhood trauma. Their plan could involve: chelation therapy or natural chelators for mercury; high-dose vitamin D and magnesium to correct deficiencies; an antifungal protocol to clear candida and then a probiotic + diet to repopulate good flora; and therapy or mind-body techniques for trauma. Meanwhile, anti-inflammatory support is given throughout (diet and herbs). Over months, the aim is that their immune system, now freed from fighting heavy metals and yeast and calmer from resolved trauma, will start “remembering” how to distinguish self from invader properly, leading to reduced autoimmunity.
One must note that patience and commitment are required for holistic treatments. They are not quick fixes; it might take 6-12 months to see major changes, whereas a steroid can reduce symptoms in days. However, the payoff could be long-lasting improvement and less dependency on drugs. Many patients use an integrative approach: staying on necessary medications initially, and as their root causes are addressed, working with their doctor to taper down the medications if their disease activity allows. It’s critical that any taper or discontinuation of meds like steroids or immunosuppressants be done carefully under medical supervision, as lupus can be life-threatening if uncontrolled. The ideal scenario is a partnership between the rheumatologist and the holistic practitioner (ND, functional MD, etc.), though finding such collaborative care can be challenging. Nonetheless, the patient can be the bridge, by keeping all providers informed of what they are doing and monitoring their lab tests and symptoms closely.
Lupus, Lyme, and Fibromyalgia: Different Names, Common Threads
Earlier we touched on the similarities between lupus and other mysterious chronic illnesses. It’s worth revisiting, because understanding lupus in context can help demystify it. Lyme disease and fibromyalgia are two conditions that often come up in the differential diagnosis with lupus, and indeed some patients carry multiple diagnoses over time as doctors struggle to categorize their syndrome. Each condition has its conventional definition: lupus is autoimmune with identifiable lab markers (like ANA, anti-dsDNA); Lyme disease is an infectious disease with a known microbe (Borrelia) and treatable with antibiotics (at least in the early stage); fibromyalgia is a syndrome of chronic widespread pain with no obvious inflammation or tissue destruction, thought to be a central nervous system pain processing disorder. On the surface, they seem distinct. Fibromyalgia, for instance, “doesn’t cause inflammation, swelling, or damage to bodily tissues,” whereas lupus clearly doeshealthline.comhealthline.com. And yet, the symptoms overlap a great deal: all three can involve fatigue, joint/muscle pain, brain fog, and poor sleep. A person with Lyme or lupus might meet the tender point criteria for fibromyalgia, and conversely many lupus patients (up to 25%) also have fibromyalgia as a comorbidityarthritis.orgmedicalnewstoday.com. This begs the question – are these truly separate illnesses, or points on a spectrum?
A holistic view suggests that chronic illnesses like lupus, Lyme, fibromyalgia, chronic fatigue syndrome, and even conditions like multiple sclerosis or rheumatoid arthritis, share underlying themes: immune dysregulation, chronic infection or microbiome imbalance, systemic inflammation, and often trauma or stress. The differences may lie in genetics (which tissues get targeted or how the immune system reacts), and the original trigger (a tick bite in Lyme, vs. maybe Epstein-Barr in lupus, vs. physical or emotional trauma in fibromyalgia). But ultimately, all these conditions involve the body being in a state of disharmony and overload. It’s noteworthy that Lyme disease can mimic lupus so closely that there have been misdiagnoses; indeed Lyme has been nicknamed “The Great Imitator” for its ability to resemble various autoimmune and neurological disorderslymemexico.comautoimmune.org. Cases like the one in the literature where Lyme infection triggered lupus blur the line between infection and autoimmunitypmc.ncbi.nlm.nih.gov. Similarly, fibromyalgia has been considered by some researchers to potentially have autoimmune components – recent studies found fibromyalgia patients have small-fiber neuropathy and elevated cytokines, and there is speculation that in some cases fibromyalgia might be a post-infectious or immune-mediated conditionhealthline.comhealthline.com. The Rheumatology community recognizes that fibromyalgia often co-exists with autoimmune diseases; one reason it’s important to distinguish is that treatments differ (fibromyalgia is treated with nervous system modulators like antidepressants and exercise therapy, while lupus needs immunosuppression). However, if you treat a lupus patient’s lupus but ignore their co-existing fibromyalgia, they will still feel unwell due to pain and fatigue. Thus, an integrative approach that addresses the whole person can tackle both. For instance, treating lupus with hydroxychloroquine and doing gentle aerobic exercise and magnesium supplementation could alleviate fibromyalgia symptoms in the lupus patient.
From a patient perspective, these labels can certainly be confusing and sometimes feel “it makes no sense” how they overlap. A person might say, “I have fatigue, pain, brain fog – one doctor says fibromyalgia, another is checking me for lupus, another thinks it might be chronic Lyme, but all I know is I feel terrible and no one is fixing it.” The common thread is often underlying inflammation and energy production issues. Mitochondrial dysfunction (the cells’ energy factories not working well) is another theme in these illnesses – heavy metals and infections can impair mitochondria, leading to fatigue and muscle pain regardless of the label.
The implication is that a root-cause-focused treatment could benefit all such patients, tailored to their specific triggers. Remove Borrelia infection in Lyme, remove gluten in someone whose fibromyalgia is aggravated by gluten, remove hidden EBV in lupus – and support the body’s repair in all cases. We’ve seen how detox, gut health, and stress reduction likely help not only lupus, but also chronic fatigue syndrome and even long COVID – because these interventions reduce total body stress and allow healing mechanisms to take hold. This is not to say diagnoses aren’t important – they are, especially for acute management and certain organ-specific risks (e.g., lupus affecting kidneys is very different from fibromyalgia which doesn’t damage organs). But it is to say that patients should not be siloed by their diagnosis, and doctors should cast a wide net in searching for contributors to the illness, beyond the textbook definition. Ultimately, whether it’s lupus, Lyme, or fibromyalgia, the goal is to restore the body’s natural equilibrium. Modern medicine’s failure to cure many of these chronic conditions suggests we need to broaden our approach. By integrating insights from various fields and focusing on the person (not just the disease name), we improve the chance of true healing.
Conclusion: A New Vision for Understanding and Healing Lupus
Lupus has long been one of medicine’s most challenging puzzles – a disease with myriad symptoms, unpredictable flares, and treatments that, at best, control it without curing it. The conventional approach, while lifesaving in many cases, often leaves patients feeling like they are fighting their own body indefinitely, with only partial relief. However, by looking deeper into why the immune system is behaving erratically, we uncover a more hopeful narrative: lupus is not a random act of self-destruction by the body, but rather a complex response to a burden of pathogens, toxins, imbalances, and stressors. The immune system, in essence, may be doing its best to protect us, but gets overwhelmed and misdirected in the process.
Mainstream research is gradually validating aspects of this view – recognizing, for example, that viruses like EBV can precipitate lupus, that heavy metals can break immune tolerance, that gut bacteria and permeability influence autoimmune risk, and that severe stress can ignite diseaselupus.netpmc.ncbi.nlm.nih.govmfm.auhsph.harvard.edu. These findings, often emerging from disparate fields, converge on a simple truth: the body is an interconnected whole, and lupus arises from disturbances in multiple systems. Therefore, the solution lies not in one magic pill, but in a comprehensive restoration of balance.
Naturopathic and functional medicine practitioners have pioneered this holistic approach to lupus, focusing on detoxification, immune support, and lifestyle change. While more scientific studies are needed to conclusively prove the efficacy of these methods, many patients’ stories bear out their value – stories of lupus going into remission after addressing a long-hidden infection, or after removing toxic exposures and healing the gut, or after processing deep emotional trauma. Even without the word “cure,” quality of life can improve dramatically: pain can be reduced, energy can increase, and the dosage of heavy medications can sometimes be lowered with a doctor’s guidance. For instance, targeting heavy metal detoxification has helped some patients “slow or reverse the disease process” by removing an underlying triggerdrhilarychambers.com. Similarly, adopting an anti-inflammatory diet and stress management routine has, for others, cut their flare frequency substantially. These individual successes light the way for a future where an integrative model might become the standard.
Crucially, the holistic perspective does not negate the contributions of Western medicine – rather, it builds on them. Immunosuppressive drugs and corticosteroids can be critical tools to control acute lupus symptoms and prevent organ damage; one should not abandon them carelessly. Instead, one can incorporate natural therapies alongside conventional ones, aiming to strengthen the body so that, over time, less medication is needed. This integrative strategy requires a nuanced, patient-by-patient approach and close monitoring, but it offers a path toward not just surviving with lupus, but potentially thriving. Patients often find empowerment in this approach, as it gives them proactive steps they can take (diet, detox, mind-body practices) rather than feeling entirely dependent on prescriptions.
In reevaluating lupus through the lenses of natural health, Traditional Chinese Medicine, Ayurveda, functional medicine, and more, we return to age-old principles: find the root cause, support the body’s innate healing ability, and treat the whole person. Traditional wisdom, even if it used different terminology (Qi, doshas, etc.), always sought to identify imbalances and restore harmony – something modern lupus management can greatly benefit from. And modern science, with its ability to detect viruses in tissues or measure toxin levels, provides tools to pinpoint those imbalances like never before.
So, what lies ahead? Ideally, more research will formally test integrative therapies in lupus – for example, clinical trials of gut-healing programs or heavy metal chelation in lupus patients to quantify outcomes. The anecdotal and small-scale evidence is promising, but broader validation could bring these methods into mainstream use. In the meantime, patients and practitioners willing to “look in the wrong direction” (as in, outside the mainstream dogma) continue to experiment and learn. Every person with lupus is unique; thus, the journey to wellness will look different for each. But the guiding philosophy remains: remove what harms, provide what heals, and care for the mind and spirit as much as the body.
In conclusion, lupus can no longer be seen as an unknowable “autoimmune mystery.” It is a multifactorial illness that demands a multifaceted solution. Western medicine and Big Pharma may have missed the mark by focusing too narrowly on immune suppression. By widening our view to include chronic infections, environmental toxicity, gut ecology, and emotional health, we get a fuller picture of lupus – and with it, a more hopeful outlook. The keys to understanding and overcoming lupus might very well be the things mainstream medicine has overlooked. By turning those keys – through detox, nutrition, traditional remedies, and emotional healing – we may unlock the possibility of true healing. The road is certainly challenging, but with a neutral, open-minded, and patient-centered approach, a future where lupus is not a life sentence but a reversible syndrome could be within reach.
References:
- Parks CG, et al. (2016). Environmental Exposures and the Development of Systemic Lupus Erythematosus. (Heavy metals like mercury and pollutants in lupus)pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov
- Healthline – Fibromyalgia and Lupus: Differences. (Fibromyalgia is not inflammatory or autoimmune, unlike lupus)healthline.comhealthline.com
- Harvard T.H. Chan School of Public Health – Stress, psychological trauma linked to lupus. (PTSD nearly tripled lupus risk in women)hsph.harvard.eduhsph.harvard.edu
- Vibrant Wellness – The Link Between Heavy Metals & Autoimmune Disease. (Pathogens and heavy metals contribute to autoimmunity)vibrant-wellness.comvibrant-wellness.com
- Dr. Hilary Chambers, ND – Autoimmunity and Heavy Metal Toxicity. (Mechanism of heavy metals inducing autoimmunity; detox treatment)drhilarychambers.comdrhilarychambers.com
- Me & Qi – Lupus according to TCM. (TCM view: lupus due to Heat, Yin deficiency, Yang deficiency patterns)meandqi.commeandqi.com
- Sai Ayush Ayurveda – Ayurvedic Perspective on SLE. (Lupus seen as dosha imbalance; treatments like Panchakarma, herbs)saiayushayurveda.comsaiayushayurveda.com
- Singh M, et al. (2019). A Successful Management of SLE by Homoeopathy: A Case Report. (Homeopathic treatment led to clinical recovery and negative anti-dsDNA)journals.acspublisher.comjournals.acspublisher.com
- Yehudina Y, et al. (2021). Lyme Borreliosis as a Trigger for Autoimmune Disease. (Case: Borrelia infection likely triggered SLE in a patient)pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov
- GoodRx Health – Lupus Rash in Pictures. (Butterfly rash common in lupus; affects 70–80% of patients, first sign in 20%)goodrx.comgoodrx.com
- Healthline – Lupus vs Fibromyalgia. (Lupus causes organ inflammation; fibromyalgia causes pain without inflammation)healthline.comhealthline.com
- National Institutes of Health (NIH) – Arthritis & Rheumatology (2017). (Study linking trauma/PTSD to higher lupus incidence)hsph.harvard.edu
- Vibrant Wellness – Exploring the Link Between Lyme and Autoimmune Disorders. (Lyme infection can cause molecular mimicry, chronic inflammation leading to autoimmunity)vibrant-wellness.comvibrant-wellness.com
- PubMed – Heavy Metals and Autoimmunity. (Evidence that mercury, cadmium, lead exposures can precipitate autoimmunity in susceptible individuals)pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov
- Lupus Foundation of America – What is Lupus? (Definition of lupus as autoimmune disease causing inflammation in multiple organs)lupus.org
- (Additional references available upon request for specific studies and case reports)Ian Kain
Wellness Thrive Designer
�� Phone: +52 958 115 2683
�� Email: wellness@natoorales.com
�� Visit: www.natoorales.com